The Hotspotting the Overdose Epidemic Program (“The Hotspotting Program”) is an innovative, person-centered initiative designed to identify and support individuals most at risk of opioid overdose—with the goal of predicting and preventing overdose events before they occur. Led by the Staten Island Performing Provider System (SI PPS), a division of Northwell Health, the program integrates predictive analytics, peer-led outreach, care coordination and value-based outcome to drive better outcomes for people living with substance use disorders.
Backed by multiple funding sources, including philanthropic and healthcare system support, public grants, and national initiatives, the program is a model of collaborative public health in action.
Staten Island was uniquely selected for the pilot of the program as it is one of the most socio-economically and demographically representative counties of the United States. In addition, Staten Island has disproportionately suffered from the overdose crisis. The number of overdose deaths per 100,000 on the island is much higher than the national rate and it maintains the second highest borough rate of death due to overdoses in NYC.
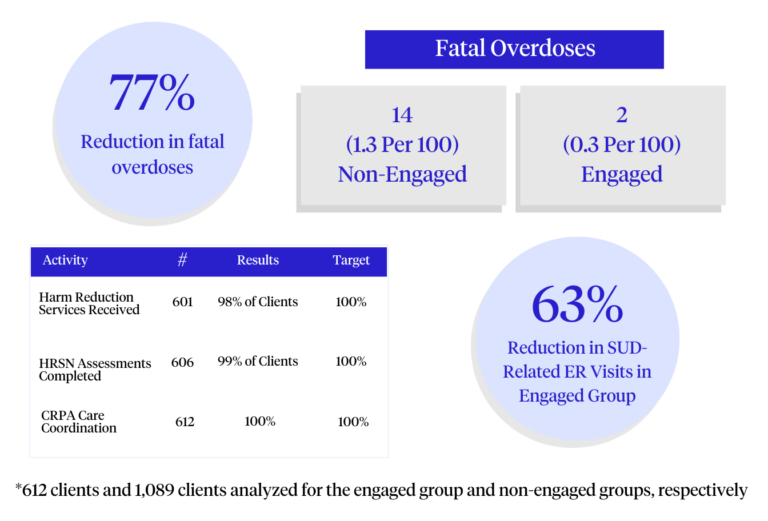
Utilizing a proven predictive analytics model developed by the SI PPS and MIT, participating entities will use data sharing arrangements to identify those most at-risk a future overdose, many of whom have been inadequately engaged in care, have left treatment programs or have been impacted by system wide issues such as a lack of access to in-person services. The Predictive analytics model incorporates 107 predictor variables and 9 outcome variables to identify this high risk population, the top 1% of which have been shown to account for more than ⅔ of future overdose events and the top 15% of which account for 90% of future overdoses within the patient sample.

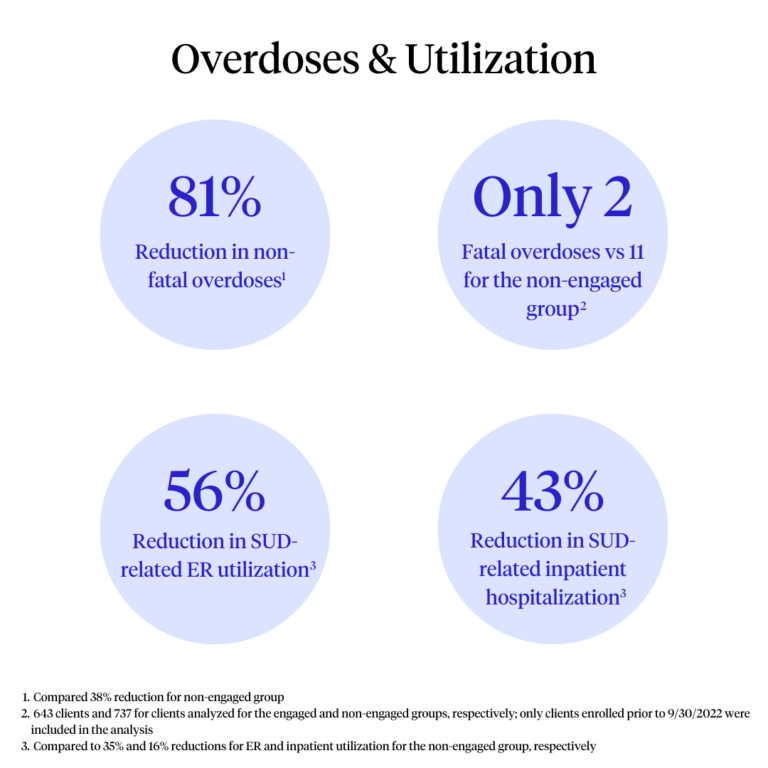
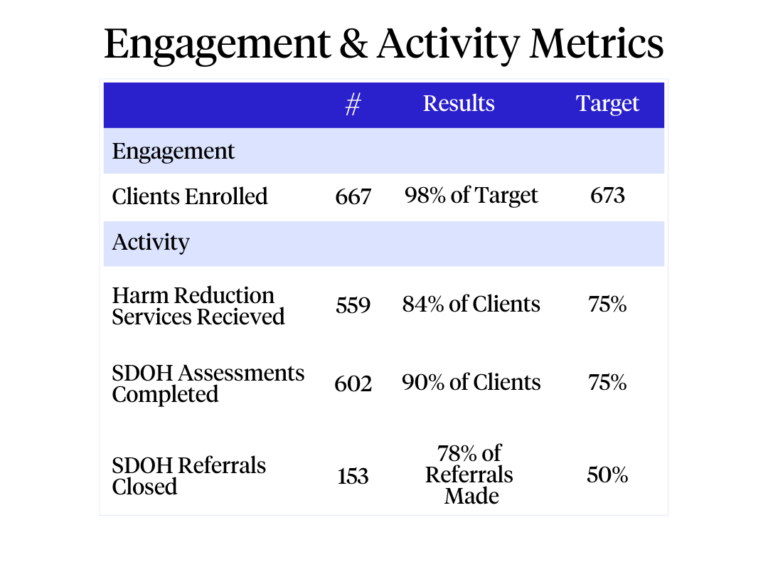
Upon identification of the high risk pool, the program places fully funded peer recovery advocates with participating treatment partners to deliver peer-led, person-centered services to at-risk individuals ‘where they are’ in a safe and collaborative manner. Dedicated teams will focus on preventing overdose harm, engaging individuals in recovery, delivering value to the health system, and addressing critical social determinants of health which impact health outcomes and lead to stressors that contribute to the initiation of an overdose, substance use disorder or relapse.
Consistent with the National Drug Control Strategy calling for evidence-based models of care, the program also incorporates Contingency Management (CM) for Medication Assisted Treatment patients. CM uses the science of behavioral economics to help individuals develop and maintain healthy habits and care plan routines. It is a proven intervention that is effective in increasing treatment retention rates, improving treatment compliance, and reducing substance use in a cost-effective way.

The Hotspotting program integrates an innovative value based reimbursement model which combines an engagement focused per member per month reimbursement rate alongside an incentive reimbursement attached to the absence of an overdose incident as well as the reduction of avoidable healthcare utilization. The program’s goal is to develop a business case for insurance companies to incentivize opioid use disorder (OUD) prevention, mitigation and treatment. All too often, managed care organizations underfund substance abuse care and maintain perverse incentives which neither benefit the patient or the system at large.
With early success in Staten Island, the program is now preparing
to scale nationally by partnering with healthcare providers, public
agencies, and Medicaid Managed Care Organizations (MCOs). As we continue to
grow, our mission remains the same: to use smart data and human connection to
prevent overdoes and save lives.
2025 Recent Expansion: NYC Health + Hospitals/Lincoln
In a major step forward, NYC Health + Hospitals/Lincoln in the South Bronx has adopted a Hotspotting program modeled on the Staten Island initiative. This pilot program, supported by a grant from the Robin Hood Foundation, aims to serve approximately 150 patients at high risk of relapse. Patients discharged from the emergency department for opioid use or nonfatal overdose will receive biweekly outreach for up to a year, connecting them to comprehensive care and support. This expansion highlights the adaptability of the Hotspotting framework and its potential to inform overdose prevention efforts across diverse healthcare settings.