The program focuses on value-based care coordination for opioid use disorder (OUD) and overdose prevention, offering a comprehensive model that combines harm
reduction, social care, and recovery support. Key components include Certified Recovery Peer Advocates (CRPAs), personalized care plans, and Contingency
Management (CM) for Medication-Assisted Treatment patients.
“The SI PPS is a very innovative program that partners with MIT to identify those at highest risk of an overdose and provide them with care when they need it most.”
Senate Majority Leader Chuck Schumer
The AI/machine learning model used to predict overdose incidents was developed in partnership with the MIT Sloan School of Management’s Initiative for Health Systems.
Participating entities use the model and data-sharing arrangements to identify those most at risk of a future overdose. The model predictor variables are motivated by known risk factors for opioid-related harm, including diagnostic codes, demographic information, provider encounters, and prescriptions filled. Training of the model was done using the SI PPS’s comprehensive database of medical claims data, electronic health records (EHR) data, and social data collected through data partnerships with emergency health, criminal justice, and social service agencies.
Upon identification of the high-risk individuals, the program places fully funded Certified Peer Recovery Advocates (CPRA) and trained clinicians with substance use disorder treatment partners to deliver peer-led, person-centered services to at-risk individuals “where they are” in a safe and collaborative manner. Harm reduction and SDOH services are essential components of the program. Central to the care management model is the notion that a CPRA should lead the engagement effort. CPRAs successfully participated in addiction recovery themselves; therefore, they can utilize their recovery experience, lived experience, and professional training to boost and support engagement in treatment and commitment to recovery for those most at risk and most difficult to engage.


Consistent with the National Drug Control Strategy calling for evidence-based models of care, the program also incorporates Contingency Management (CM) for Medication Assisted Treatment patients. CM uses the science of behavioral economics to help individuals develop and maintain healthy habits and care plan routines. It is a proven intervention that is effective in increasing treatment retention rates, improving treatment compliance, and reducing substance use in a cost-effective way.
The program utilizes alternative payment models to incentivize comprehensive and value-based care, as opposed to current fee-for-service models. It focuses on reducing harm and promotes a continuum of care leading to sustained recovery while avoiding unnecessary hospitalizations.

The Hotspotting Program demonstrated greater initial results in overdose reduction and an increase in services provided to participants in the first year of the program. There was an 81% reduction in non-fatal overdoses for those clients engaged in the program. More importantly, there were two overdose-related deaths compared to 11 in the non-engaged group. This data strongly suggests that the Hotspotting Program has had a powerful effect on overdose prevention and a significant impact on lives saved.
Although any program needs years of results to evaluate the full impact, these initial results suggest a strong impact of participation in the multiple levels of service that the program provides. Outcomes for these services include 100% of clients had a CRPA assigned to them at the initial point of engagement; from the prevention aspect, 84% of clients received harm reduction services (e.g., Narcan, an overdose reversal agent, screening for hepatitis, fentanyl test strips, and clean syringes); and from the social aspect, 91% completed screening for social care needs, with 78% of those needs met by community-based partners. The overall reduction of emergency room and inpatient care demonstrated that coordinated care can improve outcomes and ultimately impact the cost of care. A thorough analysis of visits that were specifically related to overdose and substance misuse showed that the engaged group had a reduction of 56.2% and 42.6% for ER and inpatient utilization, respectively.


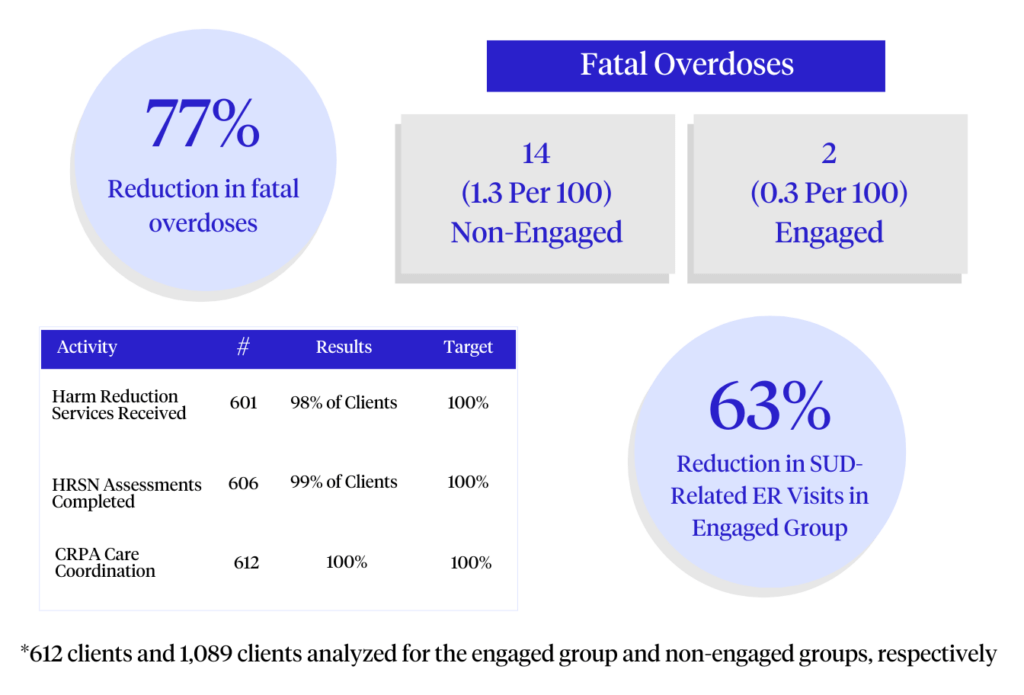
As the Hotspotting program entered its second year, the outcomes remained strong, with a 77% reduction in fatal overdoses, demonstrating a robust capacity for risk reduction in overdose fatalities. In addition, the second year saw a 63% reduction in substance use disorder-related emergency room visits, further demonstrating the program’s role in preventing crises that often lead to hospital admissions.